The risk of tick-borne infection from blood donation is hotly debated, with very little information available. Certain research studies that may clarify the risk have been done in mice but are not ethical to do in people. Meanwhile, current tests for these infections have low sensitivity and specificity (low accuracy). Consequently, it is difficult to get accurate information about the existence of infections in both donors and recipients.
Determining donor infection risk based on questions about outdoor activity has proven ineffective in real world studies. Experimental screening questions were used in an attempt to reduce Babesia species infection risk, but the questions had no effect on transfusion recipient infection rates.
Transfusion recipient infection symptoms can be complicated by their health status. This complicates accurately recording when and if a patient was infected by a blood transfusion. Recipients with a compromised immune system may show delayed or atypical symptoms. Specific illnesses may interact with tick-borne infections in other ways. For example, sickle cell disease patients may not show signs of Babesia species infection risk (babesiosis) until several months after infection.
A core concern of course is Lyme disease. In 2018 a person in Arkansas discovered she had Lyme disease and was surprised to learn that she could donate blood four weeks after the end of symptoms and treatment, per the Arkansas Blood Institute. If a donor reported suspected Lyme disease after donating, the Arkansas Blood Institute stated, “If we were given the time frame of the suspected tick bite or appearance of symptoms, we would quarantine un-transfused units or notify transfusing hospital of the risk.”
At the time, station THV11 interviewed the state epidemiologist for Arkansas. He stated that he didn’t consider Lyme disease a high risk in the state. Even in states where there is higher risk such as Connecticut or New York, current regulations do not require donated blood to be tested for Lyme disease.
Research on the risk of transmission of Lyme disease from blood transfusions has mainly been done in mice. These studies have shown that there is a risk of Lyme disease transmission in mice via blood transfusion.. However, in people a risk has not been documented. There are not high numbers of people showing symptoms of Lyme disease after receiving blood transfusions.
How is it possible to have Lyme disease and not transmit the infection in blood? Borrelia species (bacteria that cause Lyme borreliosis) often migrate to tissues in various areas around the body shortly after entering the bloodstream. Therefore, they may not actually be present in the blood when the donation occurs.
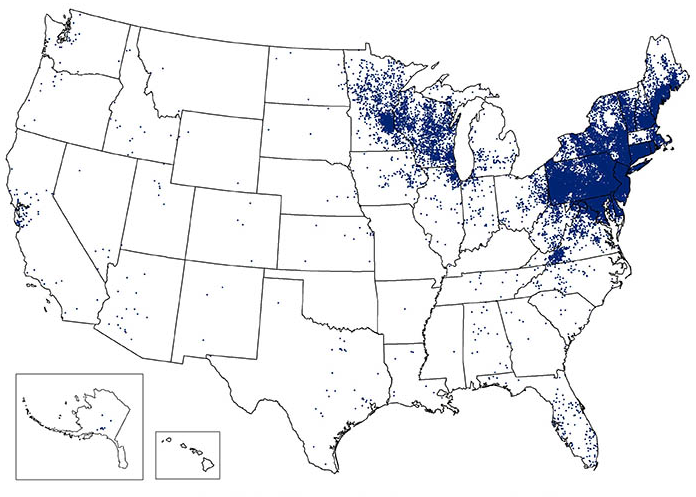
In contrast, a study of blood transfusion recipients in New York from 2004 to 2015 identified 55 cases of babesiosis linked to receiving infected blood. Transfusion-transmitted babesiosis is “the leading infectious cause of mortality (38%) in transfusion recipients…” per the American Association of Blood Banks (AABB). Unlike Borrelia species that can survive elsewhere in the body, Babesia are parasites that rely on red blood cells for survival.
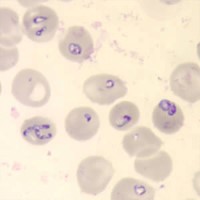
Beginning in 2012 the American Red Cross screened donors in high risk areas for babesiosis. From June 2012-May 2018 over a half a million donations were screened and 1299 were identified as positive. Blood from screened donors resulted in significantly fewer recipient infections that unscreened donations in the same region during the same time period. This experience added data to the push to screen more donors for babesiosis.
In July 2018 the FDA release a draft Guidance for Industry Recommendations for Reducing the Risk of Transfusion-transmitted Babesiosis and it was finalized in May 2019. Between the draft and final FDA guidance, the American Association of Blood Banks (AABB) issued their own Association Bulletin #14-05. A document to raise awareness, topics included:
- Shortcoming of screening questions
- Shortcoming of anti-infective blood treatments
- Encouragement to use testing as it became available, meanwhile participation in testing studies
- Symptoms of infection in blood transfusion recipients
- Best practices in treatment of infection
Meanwhile, along with Lyme disease, the risk of other tick-borne infections transmitted through blood transfusion remains an open question. Research has consistently shown that blood donors carry tick-borne infections. A study in Chile found Bartonella henselae DNA in the blood of 13.6% of blood donors tested for research. Another study of 500 healthy blood donors in Brazil found that 3.2% were PCR positive (had bacterial DNA in their blood) for at least one Bartonella species using Galaxy Diagnostics’ patented Bartonella ePCR test.
A study in Poland that focused on the risk of tick-borne disease in HIV patients but used blood donors as a control. In the blood donor group patients were found who were seropositive to each of six different tick-borne pathogens. Nine of the blood donors had been treated for Lyme disease within the past 10 years.
“Seropositive” means that they have been exposed to the pathogen (or possibly a similar pathogen that cross-reacted with the test antigen) at some point in their life. It does not necessarily mean that they are currently infected. Further research would be required to establish the link from current infection, to the presence of the infection in blood, to the ability of the pathogen to survive blood collection and current anti-infective measures which may include irradiation and UV light exposure, among other measures.
Why wouldn’t blood banks just test all blood for every possible pathogen? The difficulty is that tests for tick-borne pathogens are time-consuming and expensive. Some tick-borne disease tests would be unlikely to be completed until well after the blood is used, using current testing technology.
The cost of donor blood is sometimes placed as low as $300 per unit in the United States, however when all the costs associated with using donor blood are taken into account including blood that is prepared but not used, complications associated with transfusion, etc. the cost in 2007 was calculated at $1,158 per transfused red blood cell unit. This cost of blood has a direct impact on patients.
Conclusion
Stewards of lifesaving blood products are responsible for making it as accessible as possible while minimizing patient risk. Tick-borne disease presents an incredible challenge because determining the likelihood of infection in donors is almost impossible unless their clinical history is clear. Furthermore, diagnostics are expensive and have shortcomings that limit how thorough a screening process could be. This requires stewards to make choices about tick-borne disease risk to blood banks in an environment where there is not adequate research nor the testing tools available to meet their current needs.
References
Pawełczyk, A. et al. (2019). Seroprevalence of six pathogens transmitted by the Ixodes ricinius ticks in asymptomatic individuals with HIV infection and in blood donors. Scientific Reports, 9, 2117 [online]. doi:10.1038/s41598-019-38755-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376038/
Pitassi, LHU et al. (2015). Bartonella spp. Bacteremia in Blood Donors from Campinas, Brazil. PLoS Negl Trop Dis, 9, 1 [online]. doi: 10.1371/journal.pntd.0003467 https://www.ncbi.nlm.nih.gov/pubmed/25590435
Núñez, M. A. et al. (2017). [Prevalence of Bartonella henselae in blood donors and risk of blood transmission in Chile]. Revista Chilena de Infectologia: Organo Official de la Sociedad Chilena de Infectologia, 34(6), 539-543.[in Spanish] doi:10.4067/S0716-10182017000600539 https://www.ncbi.nlm.nih.gov/pubmed/29488546
Linden, J. V. et al. (2018). Transfusion-transmitted and community-acquired babesiosis in New York, 2004 to 2015. Transfusion, 58(3), 660-668. doi:10.111/trf.14476 https://www.ncbi.nlm.nih.gov/m/pubmed/29383735/
Wright W. (2018) Despite diagnosis, Lyme disease patients are able to give blood. THV11. 31 May 2018. https://www.thv11.com/article/news/health/despite-diagnosis-lyme-disease-patients-are-able-to-give-blood/91-560408456
Pavia, C. S., & Plummer, M. M. (2018). Transfusion-associated Lyme disease – Although unlikely, it is still a concern worth considering. Frontiers in Microbiology, 9, 2070. doi:10.3388/fmicb.2018.02070 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131610/
Centers for Disease Control, Center for Global Health Division of Parasitic Diseases and Malaria. (n.d.). Babesiosis and the U.S. blood supply [Policy brief]. Available at: https://www.cdc.gov/parasites/babesiosis/resources/babesiosis_policy_brief.pdf
AABB. (2019). Babesiosis. Available at: http://www.aabb.org/advocacy/regulatorygovernment/donoreligibility/babesiosis/Pages/default.aspx
Tonetti, L. et al. (2019). The impact of Babesia microti blood donation screening. Transfusion, 59(2), 593-600. doi:10.1111/trf.15043 https://www.ncbi.nlm.nih.gov/pubmed/30499595
Shander A. Et al. (2008). The true cost of red blood cell transfusion in surgical patients. Blood, 2008 112:3045. http://www.bloodjournal.org/content/112/11/3045?sso-checked=true


