The CDC estimates that 15% of US adults are affected by chronic kidney disease, with about 90% being unaware of their reduced kidney function. This is partially because the exact cause or trigger of kidney disease is often unknown. It could be a result of high blood pressure, autoimmune conditions, genetic susceptibility, infections, or other issues. How does bartonellosis play a role?
Bartonellosis (Bartonella species infection) can mimic autoimmune processes, often causing chronic, multi-systemic inflammation that impacts vital organs over time, including the kidneys. Kidney damage may be found after endocarditis is first identified or as a primary symptom.
More than 55 cases of Bartonella species infection associated with autoimmune kidney damage have been reported. Other symptoms of bartonellosis can also affect the kidneys. For example, an otherwise healthy 36-year-old man developed a cough that progressed into muscle pain, a rash and a fever. The cough had responded to antibiotics, but with the discovery of an autoimmune condition affecting his kidneys, he was put on immune-suppressing medications. He got worse.
Blood cultures did not reveal any kind of infection, but as he developed endocarditis he was put on a combination of antibiotics. His heart problem worsened and required surgery. Tissue taken from the heart during surgery tested positive for Bartonella henselae. The man was treated with antibiotics for bartonellosis but required ongoing treatment for the autoimmune condition.
Kidney Structure and Function
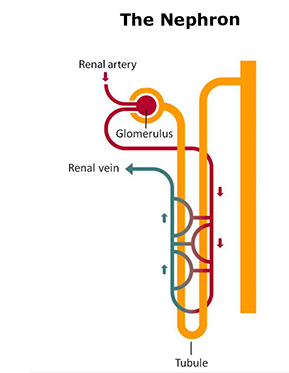
Kidneys are fairly small organs, but every day about 150 quarts of blood pass through them. Specifically, the blood passes through a tiny structure called a glomerulus that filters the blood. It then continues through a very small blood vessel that is entangled with a tubule carrying the material that was filtered out. Further transfer of material continues until the blood exits the structure.
Exactly what is transferred is controlled through an interplay of hormones produced by the kidneys themselves and by the brain. This control of materials ultimately controls blood pH and blood pressure and also impacts blood sugar levels, bone calcification, red blood cell production and more.
Cat Scratch Disease and Kidney Lesions
Cat scratch disease (acute infection with certain species of Bartonella including Bartonella henselae) can lead to inflammatory lesions in the kidneys.
One kind of lesion is called a “granuloma”. It can occur in a variety of organs including the kidneys. These lesions are caused by inflammation in response to an infection or due to an autoimmune disorder and can disrupt the function of the organ. A “necrotizing granuloma” causes regional cell death.
Another kind of lesion occurs during glomerulonephritis, when the glomerulus inside the kidney becomes inflamed. Case reports have associated glomerulonephritis with endocarditis (heart inflammation) caused by Bartonella species infection. A report from 2004 described three patients with necrotizing glomerulonephritis associated with endocarditis. After renal biopsies, two of the patients were further investigated for heart issues, leading to the discovery of their endocarditis and subsequent heart surgery. One patient died after four months from kidney failure.
Post-Transplant Complications
Cat scratch disease is often associated with inflamed lymph nodes. There is a condition called post-transplant lymphoproliferative disorder (PTLD), which is a lymphoma (lymph node cancer) that is a risk after transplant. A case report describes a kidney transplant patient being evaluated for PTLD who was found to have cat scratch disease instead.
In general, patients on immunosuppressive medications following a transplant of any kind are at increased risk of contracting bartonellosis and exhibiting atypical symptoms. Kidney granulomas as a symptom of bartonellosis are a particular risk in people with suppressed immune systems.
Vasculitis
Vasculitis is inflammation of the vascular tissue, the veins and arteries that carry blood throughout the body. It has been associated with bartonellosis and can cause symptoms throughout the body. The tiny vessels in the kidney can be especially susceptible to damage and reduced functionality from vasculitis.
Autoimmune Conditions
The connection between bartonellosis and autoimmune conditions is still poorly understood. However, bartonellosis may serve as a trigger for autoimmune conditions, particularly in people who were already genetically susceptible to a particular condition.
More than 55 cases reporting an association between bartonellosis and antineutrophil cytoplasmic antibodies (ANCA) have been published. These are often associated with endocarditis as well as kidney damage. ANCA cause an autoimmune reaction in which the body attacks its own neutrophils (a kind of white blood cell). The presence of ANCA can lead to granulomas, glomerulonephritis and/or vasculitis, including a specific kind of dangerous vasculitis in the kidneys called pauci-immune vasculitis.
Conclusion
The kidneys are responsible for efficiently removing waste from the blood and excess water from the body. When they are impacted by inflammatory processes, such as granulomas and vasculitis, they cannot do their job appropriately. There is still a lot to learn about how bartonellosis may contribute to chronic kidney disease (CKD), but research suggests that people with immune system concerns should be aware of the risk Bartonella species pose to the kidneys.
References
Shamekhi, A. F. (2017). Bartonellosis in chronic kidney disease: An unrecognized and unsuspected diagnosis. Therapeutic Apheresis and Dialysis, 21(5), 430-440. doi:10.1111/1744-9987 https://www.ncbi.nlm.nih.gov/pubmed/28884961
Bookman, I. et al. (2004). Necrotizing glomerulonephritis caused by Bartonella henselae endocarditis. American Journal of Kidney Diseases, 43(2), e8.1-e8.6. doi:10.1053/j.ajkd.2003.10.027 https://www.ajkd.org/article/S0272-6386(03)01384-2/abstract
Tandukar, S., & Wu, C. (2017, November). Disseminated bartonellosis masquerading as PTLD in a renal transplant recipient. Abstract of a case presented at the American Society of Nephrology Kidney Week, New Orleans, LA. https://www.asn-online.org/education/kidneyweek/2017/program-abstract.aspx?controlId=2762306
Chaudhry, A. R. et al. (2015). Bartonella henselae infection-associated vasculitis and crescentic glomerulonephritis leading to renal allograft loss. Transplant Infectious Disease, 17(3), 411-417. doi:10.1111/tid.12376 https://www.ncbi.nlm.nih.gov/pubmed/25753276
Vercellone, J. et al. (2018). Bartonella endocarditis mimicking crescentic glomerulonephritis with PR3-ANCA positivity. Case Reports in Nephrology, 2018, 9607582. doi:10.1155/2018/9607582 https://www.ncbi.nlm.nih.gov/pubmed/30210883
Raybould, J. E. (2016). Bartonella endocarditis and pauci-immune glomerulonephritis: A case report and review of the literature. Infectious Diseases in Clinical Practice, 24(5), 254-260. doi:10.1097/IPC.0000000000000384 https://www.ncbi.nlm.nih.gov/pubmed/27885316
Shah, S. H. et al. (2014). Touch not the cat bot a glove: ANCA-positive pauci-immune necrotizing glomerulonephritis secondary to Bartonella henselae. Clinical Kidney Journal, 7(2), 179-181. doi:10.1093/ckj/sft165 https://www.ncbi.nlm.nih.gov/pubmed/25852867
Centers for Disease Control and Prevention. (2019). Chronic kidney disease in the United States, 2019. Retrieved from https://www.cdc.gov/kidneydisease/publications-resources/2019-national-facts.html

