Opportunistic infections occur when pathogenic microbes take advantage of an abnormal situation in the body. This may be a break or weakness in a barrier like skin, a disrupted microbiome, or a weakened immune system. In some cases, opportunistic infections are caused by microbes that are part of the normal microbiome of healthy people. Let’s explore this further with Bartonella species, H. pylori, and C. difficile as examples.
Bartonella species
Some Bartonella species were discovered as opportunistic infections. Bartonella henselae infection is now typically associated with the acute presentation called cat scratch disease, but it was first identified and characterized after being isolated from HIV/AIDS patients who were experiencing severe, atypical symptoms like bacillary angiomatosis.
Bartonella quintana was first identified in hungry and exhausted soldiers living in unsanitary conditions during World War I. It is now often found in homeless populations who are at high risk for exposure to insect vectors, such as human body lice. The symptoms vary from relapsing fever to complications caused by culture-negative endocarditis.
The pathogenesis of these bacteria in chronic infections is still poorly understood. Research over the past 20 years suggests that Bartonella can affect multiple body systems when the right situation presents itself, but they can also be found in populations that are seemingly healthy and immunocompetent. For example, one study of healthy blood donors in Brazil found that 3.2% tested positive for Bartonella DNA.
You can find out more about these infections in our blog post “A Brief History of Three Diseases Caused by Bartonella.”
H. pylori
Helicobacter pylori was discovered as a bacterium associated with stomach ulcers by Drs. Marshall and Warren. They were eventually awarded the Nobel Prize for this discovery. At first it seemed that H. pylori was a villain that should be eradicated from the human gut microbiome. But the real story was more complex, as can be expected for a bacterium that has been with us for at least 60,000 years. The CDC estimates that approximately two-thirds of the world’s population is colonized by H. pylori, with the majority of people being asymptomatic.
H. pylori live in the mucosal lining of the stomach and seem to have a sweet spot. A high population within the stomach may cause problems like ulcers that lead to gastric cancer, while too little has been associated with a higher risk for esophageal conditions.
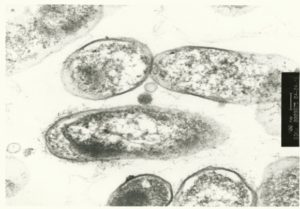
C. difficile
Clostridioides difficile (C. diff) is another bacterium that has been with us for a very long time. As many as 5% of people have it in their gut microbiome with no problems at any given time. More than 70% of babies have positive serology for C. diff by the time they are 18 months old. C. diff does not compete well against a healthy gut microbiome, so the number of bacteria stays low in a healthy baby or adult. When an antibiotic treatment weakens other microbes in the gut, however, C. diff can take over. Once it develops a colony it is even harder to kill, and it produces toxins in enough quantity to harm the host.
In the 1970s, researchers discovered C. diff was responsible for most antibiotic-associated diarrhea. In the 2000s C. diff developed antibiotic resistance as well as variants that increase their output of toxins more than 20 times. Genetic research has revealed that C. diff has been around for millions of years, but the variants that are most likely to make us sick have only been around for about 120 years.
Conclusion
Bartonella species, H. pylori and C. diff are all bacteria which have been with us for thousands of years. As they’ve co-evolved with humans, we have developed the ability when we are healthy to carry these bacteria without ill effects at least some of the time. Their stories disrupt the idea of microbes as angels or demons. Sometimes, the situation matters.
When we are sick or our microbiomes are sick, microbes that were otherwise innocuous or even beneficial may become opportunistic infections. In addition, modern pressures such as antibiotics may have altered our relationship with these microbes. In these situations, medical treatments may be necessary to restore us to health.
References
Blaser, M. J. (1998). Helicobacter pylori and gastric diseases. BMJ, 316, 1507. 10.1136/bmj.316.7143.1504 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1113159/
Heinlen, L., & Ballard, J. D. (2010). Clostridium difficile infection. The American Journal of the Medical Sciences, 340(3), 247-252. 10.1097/MAJ.0b013e3181e939d8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2935936/
He, M. et al. (2010). Evolutionary dynamics of Clostridium difficile over short and long time scales. PNAS, 107(16), 7527-7532. 10.1073/pnas.0914322107 https://www.pnas.org/content/107/16/7527
National Cancer Institute, National Institutes of Health. (2013). Helicobacter pylori and cancer. Available at: https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/h-pylori-fact-sheet
Connor, B. A. (2019). Helicobacter pylori. Available at: https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/helicobacter-pylori