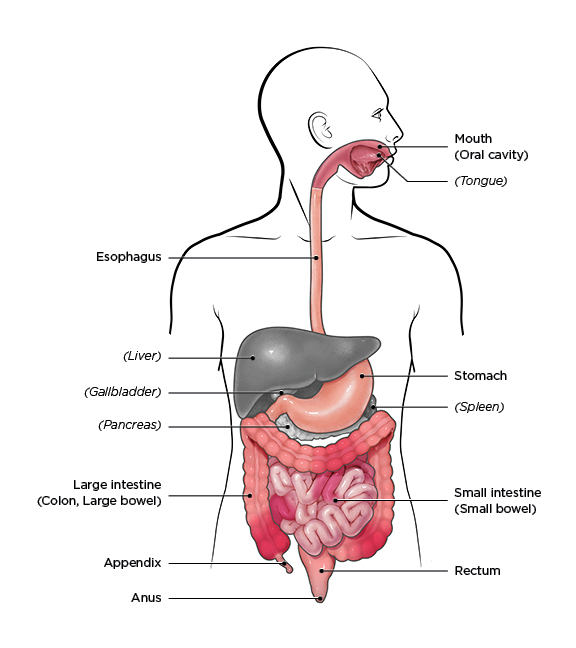
Crohn’s disease was first described in the early 1700s, but its exact cause is still unknown. It is an immune system dysregulation that is most commonly characterized by inflammation of the ileum (the final and longest part of the small intestine). However, inflammation and damage can occur in other parts of the gastrointestinal system as well as in other organs, including the skin.
In 1932, Burril Barnard Crohn and his colleagues described a series of patients with ileitis, the most common symptom of the disease, and differentiated them from other patients with inflammatory bowel conditions. Today, about 3 million people in the United States have been diagnosed with Crohn’s disease. They are mainly of Eastern European and Ashkenazi Jewish backgrounds, but diagnoses are increasing in African American people.
There are three main theories about the cause of Crohn’s disease. The first is that it is an autoimmune disease in which an overactive immune system attacks gastrointestinal tissue. The second is a more subtle version of an immune theory in which a damaged innate immune system leads to an over-expression of the adaptive immune system. The target isn’t body tissue but rather a gut microbiome that should be seen as friendly.
This leads to the third theory, which is that Crohn’s disease is triggered by an infection. One pathogen linked to this theory is a member of the Mycobacterium family known as MAP. MAP is much more common in people with Crohn’s disease than in other people, but about half of Crohn’s patients are not carriers. Clearly, MAP does not explain all cases of Crohn’s disease.
Could it be that a broader range of pathogens can trigger Crohn’s disease in those with a genetic susceptibility?
In a study of children with gastrointestinal complaints, researchers examined a larger number of pathogens than in previous studies. Bartonella species, Borrelia burgdorferi, Helicobactor pylori and Mycoplasma fermentans were found in 64% of the children, with 32% infected with more than one of these pathogens. Bartonella species were the most common infection in children complaining of abdominal pain.
Bartonella species infection (bartonellosis) has been linked to inflammatory immune system changes that can lead to a range of chronic, non-specific symptoms. In 2017, researchers described two cases of patients who experienced neurological symptoms due to immune dysregulation associated with bartonellosis.
A few other published case studies link bartonellosis and inflammatory bowel findings similar to Crohn’s disease. In 2001, doctors reported a case of ileitis in a child. Ileitis is the most common symptom of Crohn’s disease, so further diagnostic testing was pursued to determine if the child had the condition. As the testing progressed, the child continued to have a fever and then developed lesions in the liver and spleen that were suggestive of bartonellosis.
The child tested seropositive for bartonellosis, resulting in a prompt and accurate diagnosis. A follow-up letter from a group of physicians in Japan noted that diverse symptoms have been found to be associated with Bartonella species infection and that they had observed inflammatory bowel disease in children to be one of these symptoms.
In 2011, doctors reported a case of Bartonella henselae infection of a replacement aortic valve. Bartonella species infection is a common cause of culture-negative endocarditis (inflammation of the inner lining of the heart), so this was not a surprising finding. What was notable was that the case also involved inflammation of the colon, or colitis, of no known cause. It took a few weeks to test the patient for Bartonella species as physicians learned more about the patient’s past animal exposure. The patient had volunteered with a cat rescue where he was scratched by homeless cats, and he had also been scratched by his own pet kitten that had subsequently died. Bartonella henselae infection is often referred to as cat scratch disease because of this route of transmission.
Two weeks of combination antibiotic therapy did not improve his condition. It was only after heart surgery to remove the infected valve and 12 months of combination antibiotic therapy that he tested negative for continued infection. His colitis also resolved.
Conclusion
Triggers for autoimmune conditions remain poorly understood. It appears that both a genetic susceptibility and an environmental trigger are required to develop many of these conditions. Bartonellosis is associated with inflammatory bowel conditions that mimic Crohn’s disease, and it is possible that Bartonella species could be a pathogenic trigger for Crohn’s disease in certain cases. However, more research is required to understand the mechanisms behind the pathogenic causes of immune dysregulation.
References
Marks, D. J. B., & Segal, A. W. (2008). Innate immunity in inflammatory bowel disease: A disease hypothesis. Journal of Pathology, 214(2), 260-266. doi:10.1002/pagh.2291 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2635948/
Chamberlin, W. M., & Naser, S. A. (2006). Integrating theories of the etiology of Crohn’s Disease on the etiology of Crohn’s Disease: Questioning the hypotheses. Medical Science Monitor, 12(2), RA27-RA33. https://www.researchgate.net/publication/7323976_Integrating_theories_of_the_etiology_of_Crohn’s_Disease_On_the_etiology_ofCrohn’s_Disease_Questioning_the_Hypotheses
Karris, M. Y. et al. (2011). Bartonella henselae infection of prosthetic aortic valve associated with colitis. Vector-Borne and Zoonotic Diseases, 11(11), 1503-1505. doi:10.1089/vbz.2010.0169 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3216094/
Massei, F. et al. (2000). Bartonella henselae and inflammatory bowel disease [Research letters]. The Lancet, 356, 1245-1246.
Numazaki, K. et al. (2001). Bartonella henselae in inflammatory bowel disease [Correspondence]. The Lancet, 357, 1974-1975.
Cañas-Ventura, A. et al. (2011). Systemic Bartonella henselae infection and Crohn’s disease treatment with infliximab [Letter to the Editor]. Inflammatory Bowel Diseases, 18(1), E197-E198.
Fried, M. D. et al. (2004, November). Simultaneous gastrointestinal infections in children and adolescents. Practical Gastroenterology, 78-80.
Kaufman, D. et al. (2017). Neurological and immunological dysfunction in two patients with Bartonella henselae bacteremia. Clinical Case Reports, 5(6), 931-935. doi:10.1002/ccr3.977 https://www.researchgate.net/publication/316489066_Neurological_and_immunological_dysfunction_in_two_patients_with_Bartonella_henselae_bacteremia


