Testing for Lyme borreliosis can be a difficult subject for patients to approach their healthcare providers about. Educating yourself on topics to discuss beforehand may help facilitate a productive conversation regarding your symptoms and why you think testing for Lyme borreliosis is the next step.
Research on Lyme borreliosis increasingly suggests that an early diagnosis is important for treatment success. However, it may be overlooked by healthcare providers when the classic symptoms of Lyme disease are absent or if the patient’s symptoms mimic other health conditions. In many cases, it can be weeks to months before the patient is assessed for Lyme disease.
These concerns have been exacerbated by the COVID-19 pandemic. Numerous news articles and studies have highlighted that persistent, non-specific symptoms experienced by “COVID-19 long-haulers” often overlap with chronic manifestations of Lyme borreliosis. A recent article delved deeper into how genetic differences between individuals may affect the host immune response and contribute to the similar processes seen across chronic illnesses like Lyme borreliosis, chronic fatigue syndrome, and more.
A case report published February 2021 described a 67-year-old man suspected of having COVID-19 following the sudden onset of chills, fever, and headache in July 2020. A skin lesion did not appear until six weeks after the negative COVID-19 test, which prompted a dermatologist to order serology testing for Lyme disease. The test was CDC-positive for IgM and a diagnosis of Lyme borreliosis was given.
Warmer weather across the United States means people are more likely to encounter ticks and other vectors. How can you talk about Lyme borreliosis and testing with your healthcare provider?
Discuss your known or possible exposure to ticks and other vectors.
Many patients diagnosed with Lyme borreliosis do not remember being bitten by a tick, but this is often the first question asked by a healthcare provider. Ixodes nymphs, which can transmit Borrelia and other pathogens to humans, are the size of a poppy seed. A special component of their saliva also makes bites and attachment relatively painless. A tick bite may escape the patient’s notice, but there are other exposure risks that should be considered.
One important factor is the geographic area in which you live. Epidemiological research suggests that there are not only “hot spots” with large populations of ticks but also areas where ticks have microbiomes richer in harmful pathogens. If you spend time outdoors in one of these areas, such as the northeastern United States, your risk may be very high.
Other considerations include travel history and occupational risk. People who have recently traveled to a Lyme endemic area or who have jobs that require being outdoors in high risk areas should make sure their healthcare providers are aware.
Bring evidence supporting why Lyme borreliosis could explain your symptoms.
Lyme borreliosis is not a one-size-fits-all type of illness. The EM rash that is considered a classic symptom of acute Lyme disease is not always present following infection. Symptoms can vary greatly between patient populations, ranging from mild illness to severe disease that affects the heart, joints, and/or central nervous system. Symptoms can also change through the course of the illness.
Because there is limited understanding of the atypical manifestations of Lyme borreliosis, healthcare providers may not think of it as a possible diagnosis. Providing peer-reviewed publications, like review articles or case reports, can support your reasoning for Lyme disease testing. A number of these resources can be found on PubMed for free.
If your provider orders testing for Lyme borreliosis: Clarify which test(s) are being performed.
Although Lyme disease can be clinically diagnosed based on symptoms and exposure risks, many healthcare providers rely on laboratory testing to provide evidence of infection. Borrelia species are considered stealth pathogens because of their ability to evade detection. This means there is often not a “silver bullet” test for Borrelia infections. It is important to understand which test(s) a healthcare provider is ordering, and why.
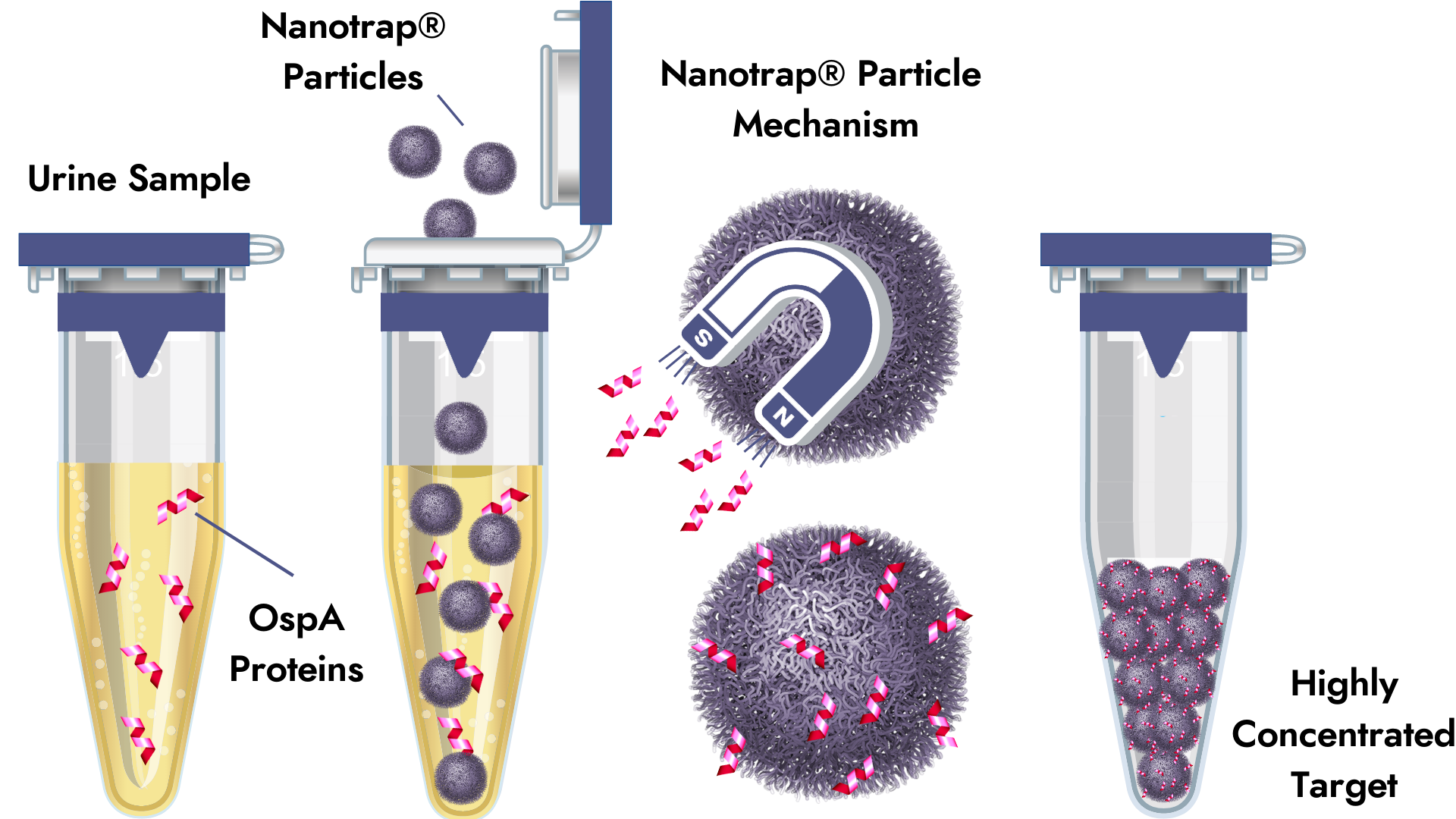
Galaxy recommends combining direct and indirect testing methods to maximize the data available for making a diagnosis. Our two-tiered testing method follows CDC-recommended criteria to determine the presence of antibodies specific to Borrelia burgdorferi in the blood, and the Nanotrap® Urine Antigen test captures the OspA protein directly from the urine. These two tests used together can provide more information than just one kind of testing.
References
Khamsi, R. (2021, April 6). The mysterious aftermath of infections. New York Times.com. https://www.nytimes.com/2021/04/06/opinion/covid-infections.html
Schlanger, Z. (2020, May 27). Lyme disease season in here. These are tips on how to avoid it. New York Times.com. https://www.nytimes.com/2020/05/27/climate/covid-coronavirus-lyme-disease.html
Stone, J. (2020, August 18). What do coronavirus and Lyme disease have in common? More than you might think. Forbes.com. https://www.forbes.com/sites/judystone/2020/08/18/what-do-coronavirus-and-lyme-disease-have-in-common-more-than-you-might-think/?sh=68fa135b37e3
Johnson, C. (2021, March 12). Study suggests similar processes are driving long COVID and ME/CFS [blog post]. HealthRising.org. https://www.healthrising.org/blog/2021/03/12/key-genes-long-covid-chronic-fatigue-syndrome/
Novak, C. B. et al. (2021). Lyme disease in the era of COVID-19: A delayed diagnosis and risk for complications. Case Reports in Infectious Diseases, 2021, 6699536. https://doi.org/10.1155/2021/6699536 https://www.hindawi.com/journals/criid/2021/6699536/?fbclid=IwAR1qTjFct11pC8gejNEkfzn3lr3vmm01UX4582MnpNHWzIB-mF0JShsUNX0
Galaxy Advanced Microbial Diagnostics. (2019, May 30). Ticks: A complex microbiome [blog post]. GalaxyDX.com. https://www.galaxydx.com/ticks-a-complex-microbiome/



