News reporting on the COVID-19 pandemic is giving the public a crash course on the transmission and pathobiology of SARS-CoV-2. A major question still puzzling researchers is what causes some people to be asymptomatic while others experience debilitating symptoms. Many clues point towards the individual’s host immune response as well as his/her ability to accommodate infection.
The global prevalence of SARS-CoV-2 has led to an enormous amount of research aimed at understanding COVID-19 on a deeper level than has been seen with many other infectious diseases. The logic used to explain the myriad of clinical manifestations, however, is applicable to unrelated diseases like bartonellosis or borreliosis. The ambiguity of COVID-19 symptoms has even been compared to Lyme disease and autoimmune disorders like lupus.
One of the most informative aspects of the COVID-19 research has been on the genetics behind disease severity. Could underlying differences in gene expression explain the differences patients report for Bartonella, Borrelia, and other vector-borne infections as well?
Host Immune Response & Genetic Predisposition
A recent news article described immunology as a “place where intuition goes to die” because of the uncertainties that immunologists face when explaining how the immune system works and what “immunity” actually means. Differences in genetics, lifestyle, and health status can all impact the host immune response. The immune system is not a “one size fits all” defensive strategy because people are not all the same. That makes it difficult to predict its behavior when exposed to pathogens, especially novel ones.
The human body has a limited number of defense mechanisms. The base of this defense is the innate immune system, which alerts the body to invaders and triggers the production of inflammatory mediators and cells. The acquired immune response organizes a more coordinated effort, creating antibodies and immune cells that specifically target and remove pathogens. The severity of symptoms, or absence thereof, is highly dependent upon how these responses play out. One drug currently used to treat severe cases of COVID-19, dexamethasone, works by mitigating the immune response rather than attacking the actual virus.
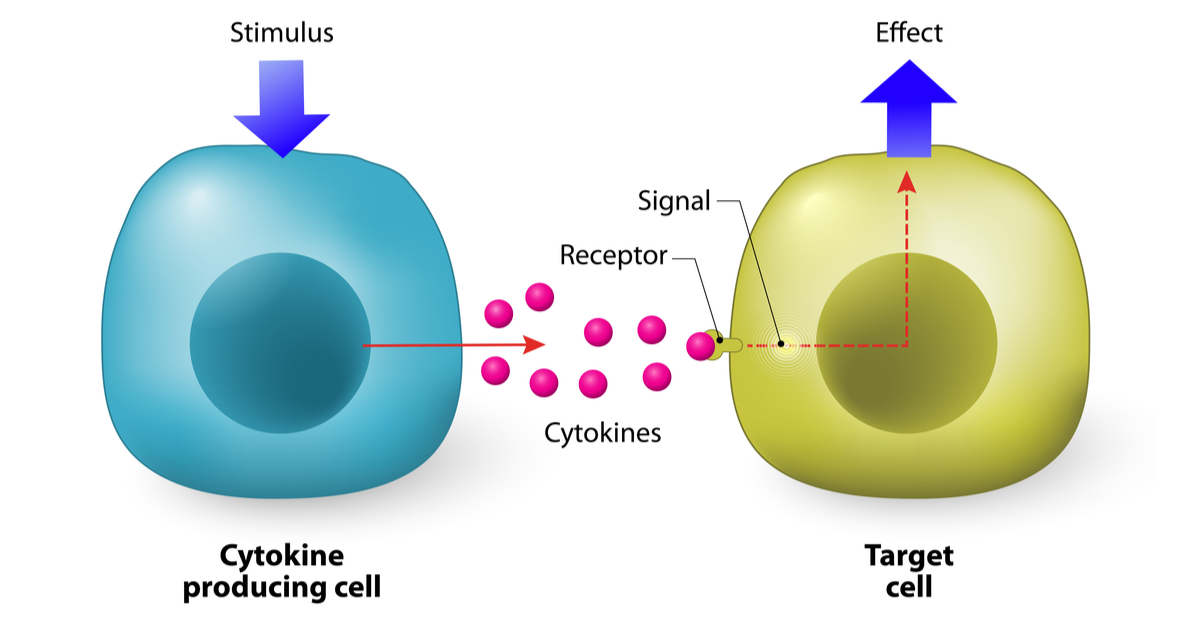
Medical professionals described a “cytokine storm” occurring in patients with life-threatening COVID-19 symptoms early in the pandemic. Cytokines act as immune mediators that can influence the host’s response to a pathogen. Research has now suggested that 14% of severe COVID-19 cases can be explained by a genetic biomarker that affects interferon, a type of cytokine.
The immune response can continue well after the infection is gone, causing ongoing symptoms. Changes in COVID-19 have been traced to changes in B cells that are seen in severe cases of lupus. These kinds of changes may be related to the fatigue and other symptoms seen in “long haul COVID” and also explain the difficulty in cases of tick-borne disease of teasing out when an infection is ongoing and when the infection may be resolved but the symptoms are ongoing.
Conclusion
Patients who suffer from under-researched diseases, including myalgic encephalomyelitis (ME), a variety of autoimmune conditions and tick-borne diseases, may benefit from the rush of research related to COVID-19. New aspects of how the immune response becomes disordered and the genetic factors that affect it have already been discovered. Treatments that benefit COVID-19 patients may end up benefiting people with a variety of other conditions as well.
References
Galaxy Advanced Microbial Diagnostics. (2020). The impact of host response on COVID-19 [blog post]. Available at: https://www.galaxydx.com/host-response-and-covid-19/
Galaxy Advanced Microbial Diagnostics. (2019). The role of host response in chronic illnesses [blog post]. Available at: https://www.galaxydx.com/the-role-of-host-response-in-chronic-illnesses/
Laber-Warren, E. (2020, August 25). The theory that could explain asymptomatic cases of COVID-19. Slate.com. Available at: https://slate.com/technology/2020/08/coronavirus-asymptomatic-disease-tolerance.html?fbclid=IwAR0XwJxlsENyJsscn4QgAnMAwDl7_W5-vWPl7DhULKwjHJZoxGO40CRQfto
Zhang, Q. et al. (2020). Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science, 370(6515), eabd4570. 10.1126/science.abd4570 https://science.sciencemag.org/content/early/2020/09/29/science.abd4570
Wadman, M. (2020). Hidden immune weakness found in 14% of gravely ill COVID-19 patients [online]. Science. 10.1126/science.abe9395 https://www.sciencemag.org/news/2020/09/hidden-immune-weakness-found-14-gravely-ill-covid-19-patients?fbclid=IwAR3pd8JdeIB48GU-E7SU8v5nPI4S9XoNmwZE6pQrAYlkkOKAOD54_y9XZAU
Yong, E. (2020, August 5). Immunology is where intuition goes to die. The Atlantic. Available at: https://www.theatlantic.com/health/archive/2020/08/covid-19-immunity-is-the-pandemics-central-mystery/614956/?fbclid=IwAR0nY9kqyRvbesjgSL8rQXxPW-OFZE5Hnei339ZUMU4LpOUOWsZhEg0gMFA
Eastman, Q. (2020, October 7). Immune cell activation in severe COVID-19 resembles lupus [news release]. Emory News Center. Available at: https://news.emory.edu/stories/2020/10/severe_covid_resembles_lupus/index.html


