Lyme disease is a tick-borne illness typically caused by spiral-shaped bacteria called Borrelia burgdorferi. It is transmitted from host species to humans primarily by ticks. The tick is known as the “vector” for the disease, thus it is a “vector-borne disease.”
Lyme disease is the most common vector-borne disease in the United States according to the CDC. It was first discovered in the mid-1970s during an epidemic of juvenile rheumatoid arthritis in Lyme, Connecticut. Since then, the number of people diagnosed with the illness has increased to an estimated 300,000 cases each year, accounting for more than 90% of all vector-borne disease in the U.S.
More than 20 species of Borrelia have been implicated in human and animal disease to date. Three genospecies of Borrelia cause most of the human disease:
- B. burgdorferi sensu stricto (s.s.) in the U.S. and Europe
- B. garinii and B. afzelii in Eurasia
Borrelia miyamotoi, first discovered in Japan in 1995, has been shown to cause Lyme-like symptoms in patients. In 2015, a series of case studies showed that patients who were seropositive for B. miyamotoi were more likely to experience joint pain and headaches. Furthermore, there is evidence for worse or more persistent symptoms when multiple Borrelia species are present. Borreliosis is a term used to describe infections with a single, or multiple, species of Borrelia.
Rarely, other species of Borrelia (B. valaisiana, B. lusitaniae, B. spielmanii, B. bissettii) have also been found in humans.
Transmission
Borrelia species are transmitted via bites from hard ticks of the genus Ixodes that live in wooded areas and grasslands at temperate climates. Ixodes ticks are typically smaller than others, making them hard to detect. Additionally, they tend to feed in hard to find places and attach painlessly due to anti-inflammatory agents in their saliva.
I. scapularis and I. pacificus are common North American vectors, whereas I. ricinus and I. persulcatus are the main Eurasian vectors. In the United States, a majority of Lyme disease cases are reported in the Northeast and Midwest. However, data from canine surveillance testing and patient report data suggest that individuals face more exposure risk than reflected in the CDC data, especially in the context of travel history and exposure to other tick species.
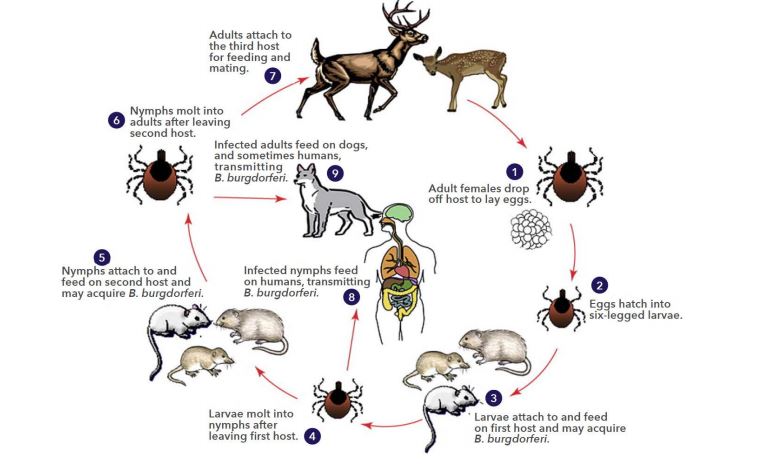
The basic Ixodes tick lifecycle involves feeding on a mammal at each life stage and then mating once the adult stage is reached (Figure 1). A common misconception is that ticks carry Borrelia species bacteria from the moment they hatch. Actually, ticks capable of hosting the bacteria (“competent” tick species) acquire the bacteria by ingesting the blood of mammalian reservoirs, like mice, as they grow from nymphs to adults.
When the tick then feeds on another animal, including humans, the bacteria can be transferred from the tick’s saliva to the skin of the new host. Borrelia bacteria then migrate through the skin until they can penetrate the blood vessels and briefly use the bloodstream as transport to other tissues and organs. Once they leave the bloodstream, they are difficult to detect.
Symptoms
Scientists in the field of infectious disease make an important distinction between infection and disease. Clinical signs associated with illness in borreliosis patients can range from hard-to-diagnose non-specific symptoms to severe symptoms affecting the heart (Lyme carditis), joints (Lyme arthritis), and central nervous system (neuroborreliosis).
Identifiable acute symptoms, like an erythema migrans (EM) rash, may appear a couple of weeks after a tick bite. The list of possible symptoms includes:
- Headache
- Fever
- Malaise
- Fatigue or chronic fatigue
- Muscle soreness
- Sleeplessness
- Depression
- Anorexia
- Fibromyalgia
- Localized or disseminated EM rash
- Joint pain
- Neurological symptoms (facial paralysis, blindness, memory loss, etc.)
- Muscle impairment, limp, or paralysis
- Arthritis
- Carditis or heart block
Risk Factors
Ticks that transmit Lyme borreliosis can be found across the United States during the spring and summer months, but are increasingly being found year round. When ticks are “questing”, or looking for a mammal to feed on, they are able to sense breath, heat, and even shadows.
They tend to wait at the ends of blades of grass or tree limbs with two appendages reaching out to attach to the next passerby. People who spend time in grassy or wooded areas are at high risk of exposure to these ticks. Animal owners also face high risk because ticks can hitch a ride on the pet and affect a person in the household later. Although these are the areas of highest risk, ticks have been found in any environment where they can be transported by animals such as birds, including beaches.
The easiest way to reduce the risk of contracting Lyme borreliosis is to follow precautions such as the ones listed below:
- Wear appropriate clothing (light colors, long sleeves, long pants, etc.) when outdoors to increase the chances of seeing a tick on you. Furthermore, reduce the amount of skin visible to decrease the likelihood of tick attachment.
- Spray clothing with 0.5% permethrin.
- Apply tick repellent that is at least 20-30% DEET.
- Perform a thorough tick check shortly after finishing outdoor activities. Areas where ticks like to attach include the scalp, bellybutton, underarms and behind the knees or ears.
- Shower, wash clothes in hot water, and dry with high heat for at least 10 minutes within two hours of arrival at home. This will reduce the chances of crawling ticks residing in the home and attaching later on.
- Give an effective flea/tick preventative to your pets year-round. The preventative should kill tick species, including Ixodes ticks, within a couple hours of attachment to reduce the likelihood of pathogen transmission. Topical tick preventatives with permethrin may help ward off ticks as well.
Diagnosis
Physicians typically diagnose and initiate treatment for Lyme disease based on a combination of clinical symptoms and results from laboratory testing, but there are some exceptions. For example, the Center for Disease Control (CDC) and International Lyme and Associated Diseases Society (ILADS) guidelines recommend starting antibiotic therapy, without laboratory evidence, if a patient presents with an EM rash. A large percentage of Lyme disease patients do not present with an EM rash, however, so physicians rely on diagnostic tests to confirm diagnoses. Organizations like the Infectious Diseases Society of America (IDSA) have also developed guidelines for physicians to follow when diagnosing Lyme borreliosis. For example, the IDSA suggests that physicians should consider the prevalence of ticks carrying Borrelia burgdorferi in the patient’s geographic region.
The CDC recommends that physicians follow a two-tier testing protocol to diagnose Lyme disease (See figure below).
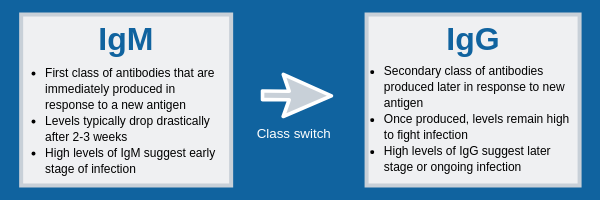
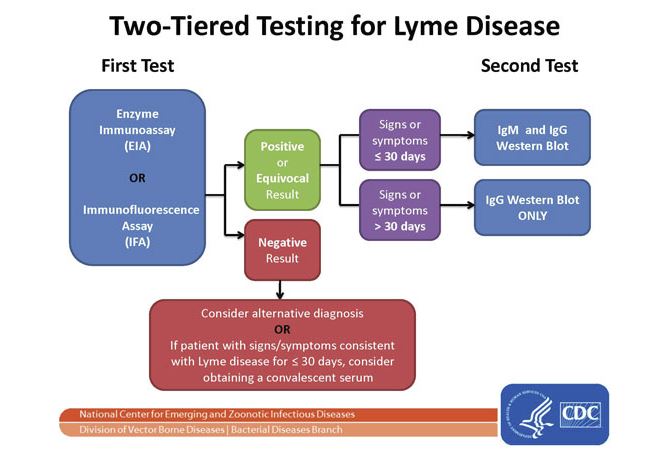 The first tier utilizes IgM or IgG-based ELISAs, or IFA, to determine if antibodies from exposure to Lyme Borrelia are present in the patient’s serum. If it tests negative, then no further testing is required. However, the physician can have a convalescent sample drawn if acute infection is strongly suspected but the IgM ELISA was negative. Patient samples that are positive or equivocal should proceed to the second tier of the protocol.
The first tier utilizes IgM or IgG-based ELISAs, or IFA, to determine if antibodies from exposure to Lyme Borrelia are present in the patient’s serum. If it tests negative, then no further testing is required. However, the physician can have a convalescent sample drawn if acute infection is strongly suspected but the IgM ELISA was negative. Patient samples that are positive or equivocal should proceed to the second tier of the protocol.
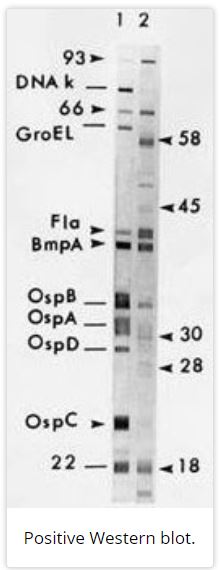
The second tier is another round of immune response testing employing IgM and/or IgG Western blot methods. A Western blot looks for antibodies that are specific to different antigens produced by Borrelia burgdorferi. The CDC criteria for a surveillance case require that an IgM Western blot sample contain antibodies that are reactive to 2 out of 3 antigens to be considered positive. An IgG Western blot requires reactivity to 5 out of 10 antigens for a positive result that meets CDC criteria for surveillance reporting.
If the results for the ELISA and Western blot are “equivocal/positive” or “positive/positive”, then the patient satisfies CDC requirements for optimal laboratory evidence of Lyme disease. However, physicians often use different testing protocols and alternate guidelines to interpret test results. There are also specialty laboratories that utilize different criteria to report positive results. Galaxy Diagnostics’ in-house two-tier Lyme disease testing follows the current CDC standards for reporting positive lab results.
What other laboratory tests are available for Lyme borreliosis?
There is an effort to develop novel diagnostic tools for Lyme Borrelia due to their increasing prevalence and incidence across the United States and the shortcomings of current testing methods. The mainstream recommended methods focus on exposure to specific species, but do not necessarily confirm active infection.
Galaxy Diagnostics offers a revolutionary direct detection test method called the Lyme Borreliosis Nanotrap® Urine Test that confirms active infection. The utilization of Nanotrap® particle (manufactured by Ceres Nanosciences) sample enrichment significantly increases the likelihood of detecting low abundance Outer surface protein (OspA) in patient urine samples.
There is also a push to develop and utilize derivatives of molecular methods, like PCR, that target Borrelia DNA in the blood, serum, and/or tissues of patients.
Treatments
Lyme disease is treated with antibiotic therapy, but the type(s) of antibiotics utilized and the duration of treatment vary with the nature of the infection and must be evaluated by a physician on a case-by-case basis.