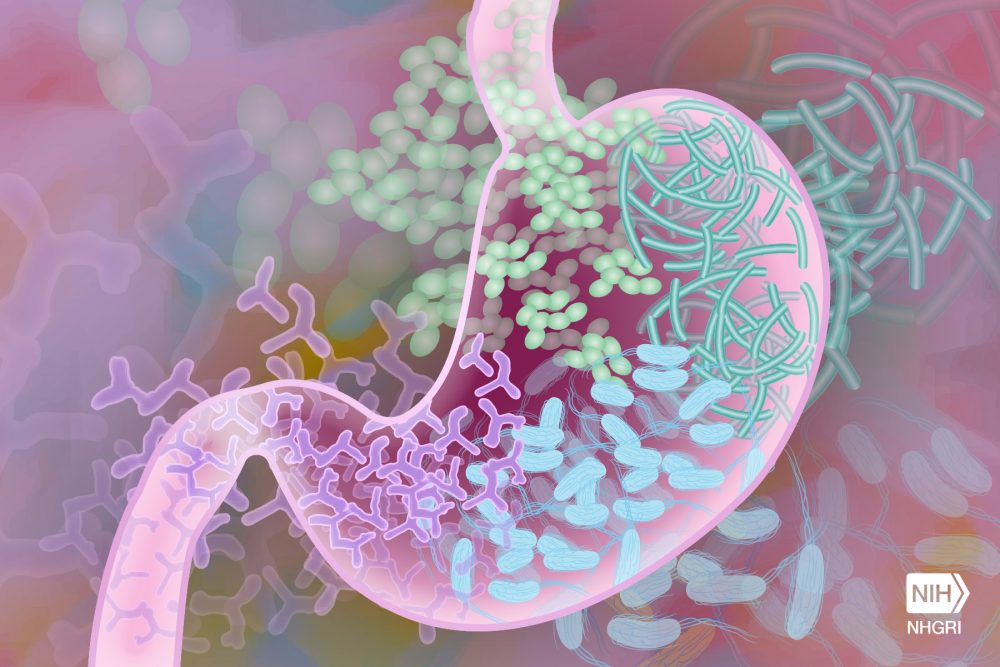
Understanding the importance of the microbiome has upended traditional thoughts about the treatment of disease. For example, treatments of autoimmune diseases that adversely affect the microbiome are being rethought. The majority of cells in the human body—cells that don’t have human DNA—are getting a new level of respect.
What are metabolites?
Despite being so different from their host’s own cells, these microbes affect the host cells dramatically even if they are in a different area of the body. Microbes in the gut can affect the brain. How do they do it? The story is multifaceted, but one chapter is metabolites.
Metabolites are small molecules that circulate in the body after they have been changed by human cells and cells from the microbiome. All of the food that you eat touches the microbiome before it is absorbed through the intestines and into the body. Pharmaceuticals are designed with the expectation they will meet the microbiome on their way to their target.
Often, the active product that affects the body isn’t the molecule in the pill that you swallow, it’s a different molecule that ends up circulating in the blood after the microbiome and the body have changed it to a metabolite. Whole categories of pharmaceuticals rely on the microbiome for their effectiveness and safety.
Metabolites and the Host Response
The role of the microbiome in influencing the host response (see our blog post on the host response) is important to how we experience diseases caused by pathogens. Part of our experience of pathogenic disease like the flu, Lyme disease or bartonellosis is damage caused by the pathogen. Another part of our experience is the host response, like fever and inflammation. The microbiome helps regulate this response.
The interplay between host cells and the microbiome starts before birth, when the mother’s microbiome affects the likelihood of a full-term pregnancy. Research on mice raised without a microbiome found that they never develop a mature immune system. The microbes that are with us from our first days are necessary to develop a healthy immune system. Specific metabolites from bacteria have been identified in the regulation of immune cell formation.
Just as pharmaceutical metabolites can have powerful effects on the body, microbiome metabolites can have effects on all the major systems of the body. Disturbances in the microbiome may play a role in inflammatory illnesses such as colitis (inflammation of the colon). Furthermore, research suggests that an unbalanced intestinal microbiome may negatively affect the brain via “leaky gut”. Increased intestinal permeability leads to metabolites entering the bloodstream and initiating inflammatory processes that could lead to neurologic symptoms. A healthy microbiome protects from inflammation.
Research on transplanted gut microbiomes in mice has found that the microbiome has an impact on their susceptibility to becoming infected with intestinal parasites. The microbiome interacted with the host to increase the host response when parasites were present.
Metabolites, Neurotransmitters and Hormones
Microbiome metabolites have effects beyond the host response, including effects on neurotransmitters and hormones. Some of the same metabolites that affect inflammation also impact signaling in the central nervous system.
How the microbiome interacts with hormone balance in the body is still being understood. Here are a couple of examples:
- The microbiome plays a key role in how soy isoflavones affect the hormonal system. Historically, more people in Asia had a microbiome that generated beneficial metabolites, but that number is falling to be more like that in the United States. This affects risks for diseases such as prostate cancer and breast cancer.
- Metformin, a drug used to treat type two diabetes, polycystic ovarian syndrome (PCOS) and other conditions, changes the microbiome. Part of its effectiveness may result from those changes.
Conclusion
Through metabolites and other modalities, the microbiome affects the host response, neurotransmitters, disease susceptibility, hormone balance and more. This impacts how we experience disease caused by pathogens and sometimes influences whether the pathogen gains a foothold at all. So much more needs to be understood about the microbiome to understand why we get sick and what treatments work to make us feel better.
References
National Institutes of Health. (2012). NIH Human Microbiome Project defines normal bacterial makeup of the body. Available at: https://www.nih.gov/news-events/news-releases/nih-human-microbiome-project-defines-normal-bacterial-makeup-body
Proal, A. D., & Marshall, T. G. (2018). Re-framing the theory of autoimmunity in the era of the microbiome: Persistent pathogens, autoantibodies, and molecular mimicry. Discovery Medicine, 25(140), 299-308. https://www.ncbi.nlm.nih.gov/pubmed/30021103
Li, H. et al. (2016). The influence of gut microbiota on drug metabolism and toxicity. Expert Opinion on Drug Metabolism & Toxicology, 12(1), 31-40. https://doi.org/10.1517/17425255.2016.1121234 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5683181/
Levy, M. et al. (2016). Metabolites: Messengers between the microbiota and the immune system. Genes & Development, 30, 1589-1598. doi:10.1101/gad.284091.116 http://genesdev.cshlp.org/content/30/14/1589.full
University of Washington Medicine Newsroom. (2019). Vaginal microbiome may influence preterm birth risk. Available at: https://newsroom.uw.edu/postscript/vaginal-microbiome-may-influence-preterm-birth-risk
Levy, M. et al. (2017). Microbiome, metabolites and host immunity. Current Opinion in Microbiology, 35, 8-15. https://doi.org/10.1016/j.mib.2016.10.003 https://www.sciencedirect.com/science/article/abs/pii/S1369527416301497
Institute of Medicine. (2013). Influence of the microbiome on the metabolism of diet and dietary components. In The human microbiome, diet, and health: Workshop summary (ch. 4). Washington, DC: The National Academies Press. https://doi.org/10.17226/13522 https://www.ncbi.nlm.nih.gov/books/NBK154098/
Caspani, G., & Swann, J. (2019). Small talk: Microbial metabolites involved in the signaling from microbiota to brain. Current Opinions in Pharmacology, 48, 99-106. doi:10.1016/j.coph.2019.08.001 https://www.ncbi.nlm.nih.gov/pubmed/31525562
Faivre, B. et al. (2019). Disentangling the effect of host genetics and gut microbiota on resistance to an intestinal parasite [Epub ahead of print]. International Journal of Parasitology. doi:10.1016/j.ijpara.2019.06.001 https://www.ncbi.nlm.nih.gov/pubmed/31525370
Lee, H. et al. (2019). Downregulation of IL-18 expression in the gut by metformin-induced gut microbiota modulation. Immune Network, 19(4), e28. doi:10.4110/in.2019.19.e28 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6722274/
Fasano, A. (2012). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy and Immunology, 42(1), 71-78. doi:10.1007/s12016-011-8291-x https://www.ncbi.nlm.nih.gov/pubmed/22109896
Mayer E. A. et al. (2015). Gut/brain axis and the microbiota. The Journal of Clinical Investigation, 125(3), 926-938. doi:10.1172/JCI76304 https://www.ncbi.nlm.nih.gov/pubmed/25689247/


