The classic description of cat scratch disease (acute Bartonella henselae infection) includes fever and lymphadenopathy (swollen lymph nodes). Additionally, an estimated 5-10% of patients develop eye-related manifestations of bartonellosis with or without the classic symptoms.
In one study of patients with neuroretinitis (inflammation of the optic nerve and retina) caused by bartonellosis, as many as 41% did not have a fever recorded by health care providers. In another study, 70% of patients had no other systemic symptoms.
Published case reports in recent years have of course included patients with fever and lymphadenopathy. When the swollen lymph node is in front of the ear on the same side as the eye and accompanied by fever it is called Parinaud oculoglandular syndrome (POGS). POGS is not uncommonly reported in conjunction with Bartonella infection that is introduced through a scratch on or around the eye.
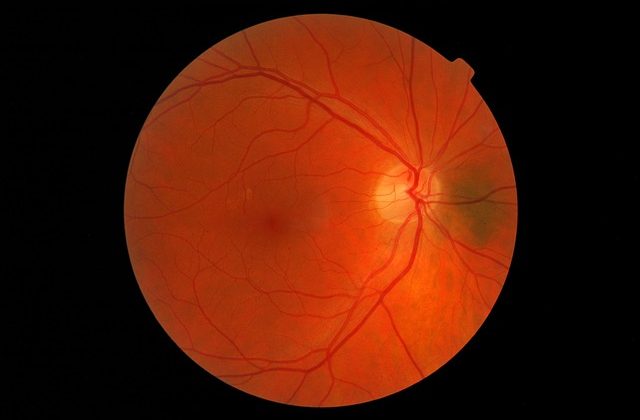
However, case reports have also been published in which the fever was not present with the neuroretinitis or occurred at a different point in the course of the disease. In some of these cases, there are only ocular symptoms such as optic disc edema or macular star, but other cases have included a spectrum of systemic symptoms including:
- Headache
- Tubulointerstitial nephritisuveitis (kidney inflammation, which with uveitis is known as TINU)
- Myocarditis (heart inflammation)
- Malaise (feeling unwell)
- Vasculitis
- POEMS Syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, skin changes)
We have previously written about the different kinds of eye symptoms that Bartonella species infection can cause, but none of these symptoms are exclusive to bartonellosis. So when should healthcare providers consider bartonellosis as a differential diagnosis?
In one reported case, a patient had eye symptoms for 10 years before being treated for bartonellosis and improving. In that case, the patient had another condition which partially explained their symptoms. Clearly the question of when bartonellosis is clinically relevant can be very complex, making it important for patients and clinicians to also consider the exposure risks for Bartonella species
Additional research about eye-related manifestations of bartonellosis and accompanying symptoms in specific patient populations should better answer the question of when Bartonella infection is relevant in the case of blurry vision, eye redness, and clinically diagnosed symptoms. Until then, one thing that has become clear is that lack of fever and lymphadenopathy is not a reason to rule out bartonellosis.
References
Gan, J. J. et al. (2011). Suspecting optic neuritis, diagnosing Bartonella cat scratch disease. Archives of Neurology, 68(1), 122-126. 10.1001/archneurol.2010.345 https://jamanetwork.com/journals/jamaneurology/fullarticle/802010
Carithers, H. A. (1985). Cat-scratch disease. An overview based on a study of 1,200 patients. American Journal of Diseases of Children, 139(11), 1124-1133. 10.1001/archpedi.1985.02140130062031 https://pubmed.ncbi.nlm.nih.gov/4061408/
Kalogeropoulos, C., et al. (2011). Bartonella and intraocular inflammation: A series of cases and review of literature. Clinical Ophthalmology, 5, 817-829. 10.2147/OPHT.S20157 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3130920/
Spinella, A. et al. (2012). Beyond cat scratch disease: A case report of Bartonella infection mimicking vasculitic disorder. Case Reports in Infectious Diseases, 2012, 354625. 10.1155/2012/354625 https://www.hindawi.com/journals/criid/2012/354625/
Ab Kahar, M. E. P. I. et al. (2020). Bartonella henselae neuroretinitis: A rare coinfection in POEMS syndrome. Turkish Journal of Ophthalmology, 50(6), 371-376. 10.4274/tjo.galenos.2020.83873 https://pubmed.ncbi.nlm.nih.gov/33389938/
Chappell, M. C. et al. (2011). Spotting Bartonella-associated uveitis. Review of Ophthalmology. Available at: https://www.reviewofophthalmology.com/article/spotting-bartonella-associated-uveitis
Ksiaa, I. et al. (2019). Update on Bartonella neuroretinitis. Journal of Current Ophthalmology, 31(3), 254-261. 10.1016/j.joco.2019.03.005 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6742623/