Vector-borne diseases like bartonellosis and Lyme borreliosis require the transfer of pathogens from a reservoir to humans by a “competent” vector.
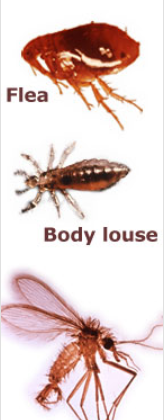
A competent vector can acquire, carry, and pass on the living pathogen. The vector is generally an insect or arthropod that picks up the pathogen(s) while feeding from a reservoir species, such as deer or mice, and later infects an accidental host (a host that is not the usual reservoir) such as a human via a bite or excretions (feces).
Despite what may seem like an obvious cause and effect relationship, it can be very difficult to prove that a vector is competent. Some scientists have heroically proven vector competency by infecting themselves. You can read more about scientists who died as a result of making themselves their own Bartonella experiments here.
Because of the work of those scientists and others, we know that Bartonella bacilliformis is transmitted by keds (biting flies), Bartonella quintana is transmitted by body lice, and Bartonella henselae is transmitted by fleas. After that the science becomes more uncertain.
The most controversial vector for Bartonella species is hard-bodied ticks of the genus Ixodes. PCR-based assays that detect fragments of DNA have shown that Bartonella bacteria can be found in their gut. However, the research on how viable bacteria are transmitted is still incomplete.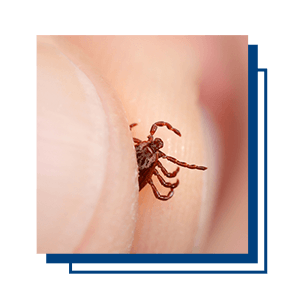
In one study of Ixodes ricinus collected in France, the authors were able to show that Bartonella henselae could be transmitted using an artificial feeding method. If one were to question whether this were adequate proof, the question would center around the fact that the transmission was observed in a controlled laboratory setting and not in nature.
Patients with Bartonella and other tick-borne infections sometimes recall a single tick bite that may have allowed for multiple pathogens to be transferred. Some scientists see this evidence as circumstantial as well and suggest more research is necessary before ticks are considered a competent vector for Bartonella.
Research and case studies have suggested additional arthropod vectors such as ants, mites, spiders, and more. They are not typically suspected in bartonellosis cases due to the very limited number of cases, but the potential is there. See below for some interesting cases:
- Spiders
- A family that lived in a house infested with woodlouse spiders became ill from Bartonella infections. Researchers suggested that the spiders were feeding on woodlice, which are also known as roly-polies or pill bugs but are actually land-dwelling crustaceans and not bugs at all. Woodlice have been shown to carry Bartonella species. Researchers suspected that the spiders fed on the infected woodlice and then transmitted the bacteria to the patients via bites.
- Red ants
- A man was hospitalized for encephalopathy due to a Bartonella henselae infection following red ant bites. While in the hospital, he experienced two episodes of cardiac arrest. He recovered after receiving systemic anticoagulatory medications and antimicrobials.
- Triatomines or “Kissing bugs”
- These biting insects are known to transmit the protozoa Trypanosoma cruzi, which causes Chagas disease. The authors of this paper discuss the role of the sand fly in transmitting Bartonella bacilliformis and suggest Bartonella species could be similarly transmitted in the saliva of other biting insects.
- Mites
- Some studies suggest various species of mites as possible vectors of Bartonella species. DNA from Bartonella quintana was incidentally discovered in Demodex mites of a patient with rosacea. Furthermore, mites found on tropical rats and bats showed evidence of carrying Bartonella species as well.
The development of novel molecular techniques like PCR and its variations have allowed researchers to detect Bartonella species in a wide range of insects, arthropods and crustaceans around the world.
Our ePCR technology is used by research partners around the world to better understand the One Health relationship between people, animals and the environment. Mapping the relationship between reservoirs, vectors and human and animal hosts is an important step in making prevention the best treatment.
References
Bradley, J. M. et al. (2014). Bartonella henselae infections in an owner and two Papillon dogs exposed to tropical rat mites (Ornithonyssus bacoti). Vector Borne and Zoonotic Diseases, 14(10), 703-709. doi:10.1089/vbz.2013.1492 https://www.ncbi.nlm.nih.gov/pubmed/25325313
Cotté, V. et al. (2008). Transmission of Bartonella henselae by Ixodes ricinus. Emerging Infectious Diseases, 14(7), 1074-1080. doi:10.3201/eid1407.071110 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2600320/
do Amaral, R. B. et al. (2018). Molecular detection of Bartonella spp. and Rickettsia spp. In bat ectoparasites in Brazil. PLoS One, 13(6), e0198629. doi:10.1371/journal.pone.0198629 https://www.ncbi.nlm.nih.gov/pubmed/29870549
Guru, P. K. et al. (2018). A miraculous recovery: Bartonella henselae infection following a red ant bite. BMJ Case Reports, 2018, bcr-2017-222326. doi:10.1136/bcr-2017-222326 https://www.ncbi.nlm.nih.gov/pubmed/29728431?fbclid=IwAR0hoMRFwoz5jVPlepkpigJ6A0zuHWrRoRy4vhNIHxNPtEotjXwqrj6NRa4
Hofmeester, T. R. et al. (2018). Role of mustelids in the life-cycle of ixodid ticks and transmission cycles of four tick-borne pathogens. Parasites & Vectors, 11(1). doi:10.1186/s13071-018-3126-8 https://www.ncbi.nlm.nih.gov/pubmed/30458847
Mascarelli, P. E. et al. (2013). Bartonella henselae infection in a family experiencing neurological and neurocognitive abnormalities after woodlouse hunter spider bites. Parasites & Vectors, 6, 98. doi:10.1186/1756-3305-6-98 https://www.ncbi.nlm.nih.gov/pubmed/23587343
Murillo, N. et al. (2014). Bartonella Quintana detection in Demodex from erythematotelangiectatic rosacea patients. International Journal of Infectious Diseases, 29, 176-177. https://doi.org/10.1016/j.ijid.2014.07.021 https://www.ijidonline.com/article/S1201-9712(14)01606-3/fulltext
Viera, C. B. et al. (2018, November). Triatomines: Trypanosomatids, bacteria, and viruses potential vectors? Frontiers in Cellular and Infection Microbiology [Online]. doi:10.3389/fcimb.2018.00405 https://www.ncbi.nlm.nih.gov/pubmed/30505806