Bartonellosis is an infectious disease caused by bacteria in the genus Bartonella. Bartonellosis causes similar disease manifestations in cats, dogs, horses, humans and potentially other wild and domestic animals. Popularly known as the key agents causing cat scratch disease (Bartonella henselae) or trench fever (Bartonella quintana), Bartonella species are very difficult to detect in patient blood, cerebrospinal fluid, joint fluid or tissue samples. Consequently, little has been known until recently about the pathogenesis of this disease. Bartonella (with over 30 named species and 17 Candidatus spp.) were essentially rediscovered in the 1990’s as a cause of vasoproliferative tumors, endocarditis and fever of unknown origin in immunosuppressed or immunocompromised (HIV) patients. Recent medical findings suggest that, while potentially life-threatening to immunosuppressed patients, bartonellosis is associated with chronic illness in immunocompetent patients. Animal and human bartonellosis has been documented in many regions throughout the world.
How do people get bartonellosis?
Bartonella species may be transmitted by contact with flea and louse feces, ticks or biting flies, or by the scratch or bite of an infected animal, most often a flea-infested cat. Bartonella species DNA have been found in several arthropod vectors in the United States, including cat fleas (Ctenocephalides felis) and ticks (Ixodes scapularis, Ixodes pacificus). Suspected transmission of Bartonella species following the bite or scratch of wild animals, such as groundhogs, squirrels and coyotes has also been documented.
Research suggests that people who live and work with animals, especially veterinary workers, have the highest risk of Bartonella infection.
Where do most cases of bartonellosis occur?
Bartonella infections in humans and animals have been documented throughout the United States and in countries in all major regions of the world. Geographic evidence suggests that prevalence of Bartonella species in arthropod vectors (fleas, ticks, lice, biting flies, etc.) is higher in warmer climates.
What are the symptoms of bartonellosis?
Bartonella species induce chronic intravascular and intracellular infection resulting in a wide range of symptoms that can include pathology involving multiple organ systems. The early clinical presentation of bartonellosis is often nonspecific with symptoms that resemble many other infectious and non-infectious diseases. Three important components of the initial clinical presentation are fever, swollen lymph nodes and at-risk exposure to arthropod vectors or bacteremic animals. None of these symptoms may be present in patients seeking medical care for chronic bartonellosis.
Symptoms that vary in number and severity among patients may include: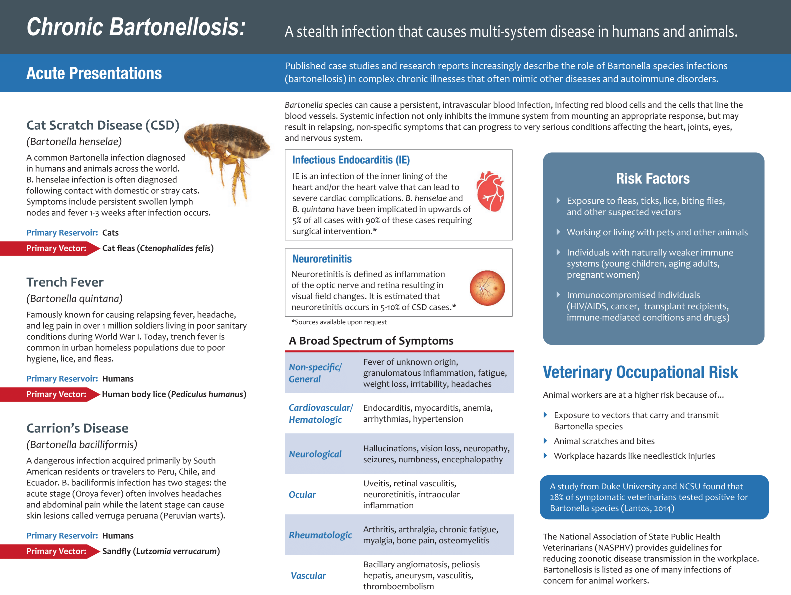
- fever
- fatigue
- headache
- malaise
- swollen lymph nodes
- skin rash or markings
- joint aches and swelling
- cardiovascular signs
- neurovascular inflammation
- abnormal sleep patterns
- memory loss
- skin lesions
- vasoproliferative tumors (Bacillary angiomatosis and peliosis)
- osteomyelitis
Bartonellosis is associated with complex disease processes in both people and animals. It is possible to be chronically infected with Bartonella and not have disease symptoms. The extent to which persistent infection in outwardly healthy individuals ultimately contributes to organ system pathology is unknown. Bartonellosis can range from severe life-threatening illnesses (myocarditis, endocarditis, vasculitis) to chronic intermittent and often relapsing symptoms listed above. It is possible that some individuals may become infected and not develop disease. It is not known if this is because some immune systems clear the Bartonella infection or because the infection is well tolerated.
How is bartonellosis diagnosed?
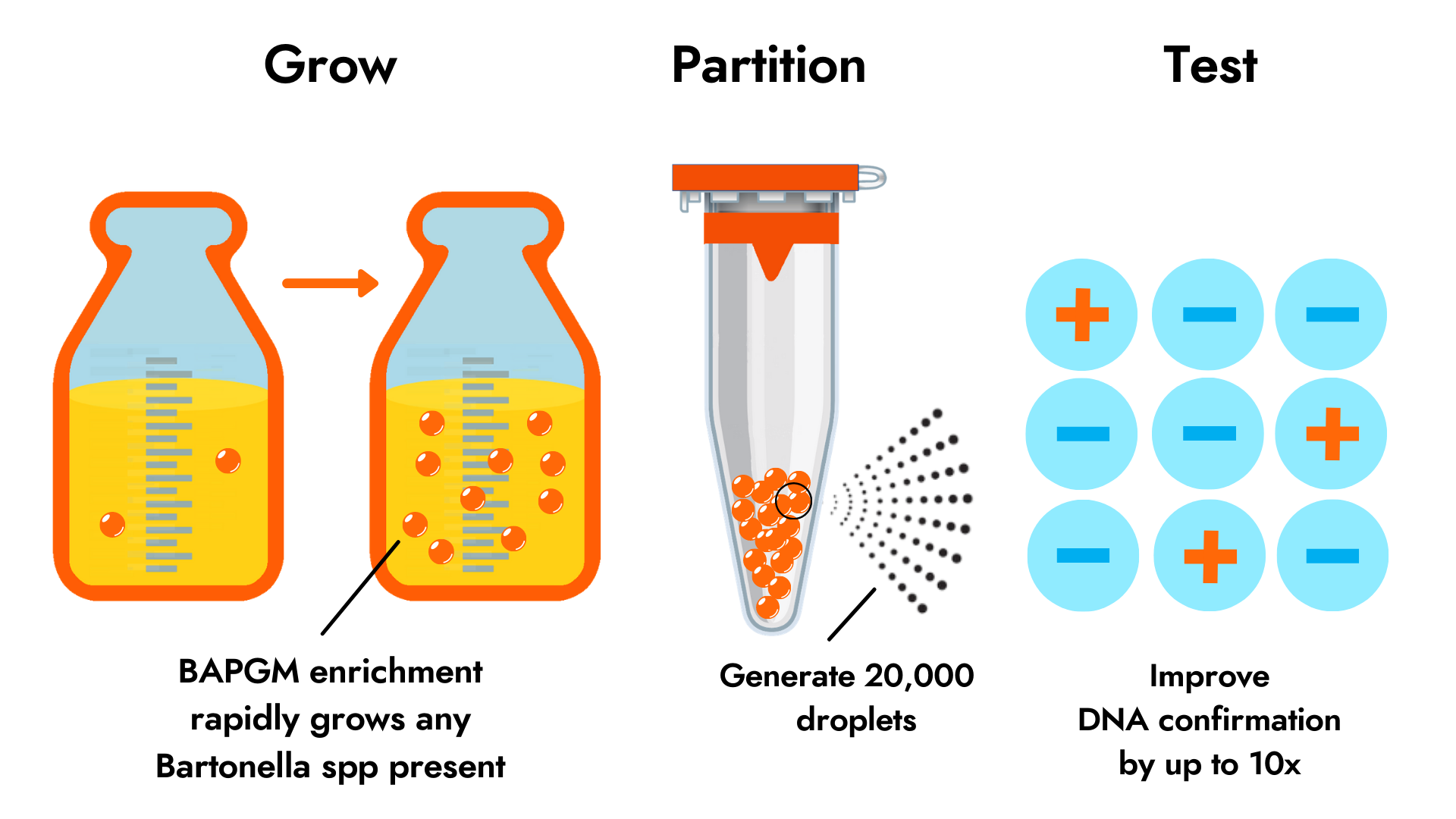
A diagnosis of bartonellosis is based on a combination of symptoms, physical examination findings and specialized confirmatory laboratory tests. Detection of Bartonella is extremely challenging, as these bacteria are immune-evasive and infect at exceedingly low levels of detection. IFA serology tests are available for the detection of antibodies, but only for a few Bartonella species. Although highly insensitive, IFA serology tests can provide evidence of exposure, but do not confirm infection. The most effective means of detecting active infection involves the combination of culture and PCR detection methods–referred to as enrichment PCR or ePCR.
Evolving evidence suggests that early detection and confirmation of Bartonella species infection (provided through Bartonella testing) is important for providing the best patient care.
Galaxy’s Advanced Test Offerings
The Bartonella Digital ePCR™ test panel is designed to detect a broad range of Bartonella species DNA. This platform combines highly sensitive genus-level ddPCR with a proprietary sample enrichment step that grows the bacteria to detectable levels. Bartonella species infect at very low levels and are, therefore, difficult to detect using conventional testing methods.
Bartonella IFA Serology (IgG) determines the presence or absence of antibodies in serum of two of the most common Bartonella species that cause disease in people: B. henselae and B. quintana. We also target B. vinsonii berkhoffii and B. koehlerae because of their potential role in chronic illnesses affecting veterinarians and other animal health workers.
Antibody levels are generally considered to be indicative of an individual’s immune response to a particular species of pathogen. The presence of antibodies may indicate that a patient has been exposed to these particular species of Bartonella.
Are there special requirements for this test?
Antimicrobial treatments may increase or decrease test targets in patient samples. However, in the absence of scientific data, we are unable to provide guidance on how these treatments may affect PCR test methods. We leave this up to the discretion of the practitioner ordering the test who may consider if the clinical situation warrants any change in treatment before testing. Unless specifically directed by the practitioner ordering the test, do not change your treatment regimen before testing.
Further Reading
Bartonellosis: One Health Perspectives for an Emerging Infectious Disease. Breitschwerdt EB. ILAR J (2014) 55 (1): 46-58. http://ilarjournal.oxfordjournals.org/content/55/1/46.full
Bartonella spp. bacteremia and rheumatic symptoms in patients from Lyme disease-endemic region. Maggi RG, Mozayeni BR, Pultorak EL, Hegarty BC, Bradley JM, Correa M, Breitschwerdt EB. Emerg Infect Dis. 2012 May;18(5):783-91.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3358077/
Neurological Manifestations of Bartonellosis in Immunocompetent Patients: A Composite of Reports from 2005–2012. Breitschwerdt EB, Sontakke S, and Hopkins S. Journal of Neuroparasitology 2012;Vol 3:1-15. http://www.ashdin.com/journals/jnp/235640.pdf
Bartonella, a common cause of endocarditis: a report on 106 cases and review. E. S., Nabet C, Lepidi H, Fournier PE, Raoult D. J Clin Microbiol. 2015 Mar;53(3):824-9. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4390654/