The Jarisch-Herxheimer reaction (JHR), or “herxing”, was first described by physicians in the late 1800s. Patients who experience this phenomenon report an increase in non-specific symptoms shortly following initiation of antibiotic treatment. These symptoms include chills, fever, headache, and/or intensification of skin rashes. Despite being described more than a century ago, it is still difficult for researchers and physicians to explain the pathogenic mechanisms that lead to JHR and the variations in patient susceptibilities.
Dr. Adolf Jarisch and Dr. Karl Herxheimer, Austrian and German dermatologists respectively, are credited with being the first to describe JHR in syphilis patients. They noted that syphilis-related skin lesions worsened soon after starting treatment with mercurial compounds. After a couple of days, the lesions would then begin to resolve. At the time, it was unclear whether the presence of mercury or something else could be causing the initial negative reaction
When penicillin, a safe and effective antibiotic, entered the market in the 1940s, it quickly became the go-to treatment for syphilis infections. However, a percentage of patients still reported an exacerbation of symptoms within 24 hours of starting treatment. Furthermore, a variety of newer antibiotics that are now commonly used, including tetracyclines, clarithromycin, and azithromycin, have been shown to provoke a JHR in cases of Lyme disease, leptospirosis, and tick-borne relapsing fever (TBRF). A case report from 2015 describes a woman who was CDC-positive for Lyme disease who had to discontinue doxycycline treatment after experiencing JHR symptoms that included facial flushing and malaise.
What causes JHR?
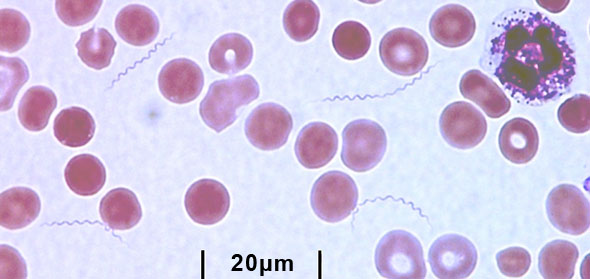
The common thread that connects syphilis, Lyme disease, leptospirosis, and TBRF is the fact that they are all caused by bacteria belonging to the spirochete family. The spirochete family is relatively small, but these corkscrew-shaped bacteria have a tremendous impact on human lives. Borrelia burgdorferi, the causative agent of Lyme disease, is currently perhaps the most well-known spirochete because of its growing prevalence. Syphilis is caused by Treponema pallidum and is sexually transmitted between people.
Research suggests that there are two main reasons that antibiotic treatment might trigger JHR in some patients.
Cellular Components
Clinicians first suspected that there may be an endotoxin in spirochetes that is released into the body once die-off begins. Many bacteria, such as Bacillus anthracis (anthrax), produce these types of toxins as a defense mechanism. However, these spirochetes were found to not have toxins that were with biologically active in humans. Instead, researchers found that unique components of the cells that remain may trigger inflammatory responses.
In T. pallidum, lipoproteins (cell surface proteins) were found to stimulate production of tumor necrosis factor (TNF) in human macrophages. Production of TNF can lead to an unnecessary inflammatory response that results in damaged muscle and other tissue. Outer surface protein A (OspA) in Borrelia burgdorferi, one of the targets of the Western blot test, has been shown to increase cytokine response in cell cultures. In 2019, researchers identified a major cell wall component, peptidoglycan, as a possible contributing factor to lasting Lyme arthritis.
Elevated Immune Response
The host immune response and mediators of inflammation, including cytokines, histamine, and white blood cells, have all been implicated in the JHR. Research suggests that treating with antibiotics can result in a short-term immune response that can cause issues for some patients.
Studies of Borrelia burgdorferi and other Borrelia species indicate that white blood cells can cause an increased inflammatory response following ingestion of the bacteria. A receptor in white blood cells can trigger a cytokine response that results in inappropriate inflammation elsewhere. Cytokines, like IL-6 and IL-8, have been shown to increase within 2 hours of penicillin treatment for relapsing fever. Furthermore, JHR may be caused by apoptosis of white blood cells (programmed cell death) after they consume Borrelia cellular products.
JHR vs. Other Treatment Symptoms
JHR-like reactions have been reported in the treatment of infections that are not spirochetes. In particular, some patients with Bartonella species infections report feeling a worsening of symptoms when they start antibiotic treatment. What is going on? These treatment symptoms have not been well-studied, but evidence is building that antibiotics have a wide variety of effects on the body. Some of the causes may be similar, such as an increase in cellular waste products from both the target bacteria and host immune cells. They may affect the host itself, changing the functioning of host cells. They also change the microbiome, causing sudden shifts in the metabolites the host cells are receiving. And of course, some of the cells in that microbiome are themselves spirochetes.
In 2017, a case study of a man who had Bartonella quintana with bacillary angiomatosis and HIV reported that during treatment he experienced immune reconstitution inflammatory syndrome (IRIS) and a JHR. These reactions developed as he was administered antiretroviral therapy for the HIV and antibiotics for the bartonellosis. The author states that the patient experienced a JHR in the form of a rash within a day of initiating treatment and then more extreme symptoms about two days after antibiotics were discontinued. Although spirochetes are typically implicated in JHR, there is evidence that other families of bacteria cause similar reactions when the patient’s microbial burden is high. This case report is free to read on the internet.
Conclusion
It isn’t uncommon for patients treated with antibiotics to report feeling worse before they feel better. These symptoms have been most closely studied in syphilis patients, leading to a variety of theories about the causes when the infecting agent is a spirochete. Yet despite more than 100 years of observation, the exact causes of treatment symptoms have not been identified even in the case of spirochetes.
References
Butler, T. (2017). The Jarisch-Herxheimer reaction after antibiotic treatment of spirochetal infections: A review of recent cases and our understanding of pathogenesis. The American Journal of Tropical Medicine and Hygiene, 96(1), 46-52. doi:10.4269/ajtmh.16-0434 https://www.ncbi.nlm.nih.gov/pubmed/28077740
Kadam, P. et al. (2015). Delayed onset of the Jarisch-Herxheimer reaction in doxycycline-treated disease: A case report and review of its histopathology and implications for pathogenesis. The American Journal of Dermatopathology, 37(6), e68-74. doi:10.1097/DAD.0000000000000093 https://www.ncbi.nlm.nih.gov/pubmed/25033009
Centers for Disease Control and Prevention. (2015). 2015 sexually transmitted diseases treatment guidelines: Syphilis. Available at: https://www.cdc.gov/std/tg2015/syphilis.htm
Jutras, B. L. et al. (2019). Borrelia burgdorferi peptidoglycan is a persistent antigen in patients with Lyme arthritis. Proceedings of the National Academy of Sciences of the United States of America, 116(27), 13498-13507. https://doi.org/10.1073/pnas.1904170116 https://www.pnas.org/content/116/27/13498

